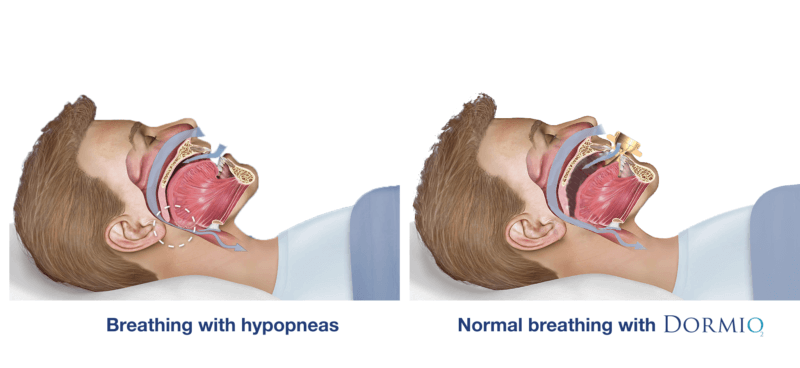
Sleep apnea syndrome is a disease characterized by partial or complete occlusion of the airway due to loosening of muscles during sleep and gravitational pulling of the tongue and/or jaw.

The complete obstruction of the airway for at least 10 seconds is called apnea, while partial obstruction of the airway related to decrease in the oxygen level is called hypopneas. The number of apneas and hypopneas can reach hundreds during the night.
The level of sleep apnea syndrome is determined by the sum of the average number of apnea and hypopnea experienced during one hour of sleep. The number of apnea and hypopnea per hour is called the apnea-hypopnea index and is called AHI for short. In the table below you can find the AHI values corresponding to the sleep apnea levels classified at three levels.

Individuals with sleep apnea are frequently ignorant of their sleep disorder. The syndrome is usually first perceived by the bed partner or cohabitant who witness the apneic episodes or it might be suspected by the clinician who notice the individual’s risk factors and symptoms.
Mostly the first indication of OSA is the complaint about patient’s snoring. With the increase in severity of the OSA, loud snoring may be associated with snorting, gasping, choking and insomnia. These nocturnal symptoms are usually underestimated by the patient until the occurrence of daytime symptoms.
Population based studies suggest that prevalence in the middle-aged adult population is currently reported at 17% of men and 9% of women. These figures apply only to the people who have been diagnosed. However, it is believed that undiagnosed OSA patients comprise an additional 5% of the general population.

Risk Factors:
Obstructive sleep apnea syndrome is strongly related to obesity and age. increased volume of the pharyngeal fat deposits is major contributor to the airway compression. Excessive fat can be accumulated under the mandible, within the soft palate and uvula. As a consequence of the deposition, the pharyngeal air space of the patient becomes narrower.
Abnormal anatomical structures can predispose pharyngeal collapse during sleep, including enlarged or elongated uvula, signs of nasal obstruction, abnormal posterior position of the maxilla or mandible, low hanging palate, unusually large tongue, enlarged lymphoid tissue and tonsils.
Sleep apnea and snoring are interconnected events. While most of the patients with sleep apnea have snoring; Sleep apnea may not be seen in every person who snores.
Snoring is the sound that occurs when the air passes through the narrowed airway and the soft tissues vibrate. Apnea, on the other hand, is when the airway completely closed by the collapsed soft tissues. For this reason, it is natural to experience snoring before sleep apnea. In a person who has just fallen asleep, airway narrowing begins with the relaxation of the tissues, as a result of which snoring is observed. Afterwards, with the deepening of sleep, apneas and hypopneas begin to be observed.
The main non-surgical treatment options for obstructive sleep apnea (OSA) are continuous positive airway pressure (CPAP) devices and oral appliances.
Sleep apnea syndrome is a disease with treatment options. The main problem here is that patients do not want to continue treatment due to device related difficulties and side effects. However, Obstructive Sleep Apnea Syndrome not only affects the quality of life but also causes more serious health problems, therefore regular treatment is necessary.
Dormio prioritizes sleep comfort and practicality while applying all of the modern treatment methods for sleep apnea syndrome. It is simply placed in the mouth like a pacifier and helps you breathe during sleep. Treatment with Dormio ceases to be a burden or torment.
Dormio keeps the tongue and jaw of the user together without any discomfort and prevents the airway from collapse by regulating intra-oral pressure with its valve system.
Dormio is designed as it will be supported by the users' lips during use in order to maintain its position.
We recommend to people who have the problem of keeping Dormio in position during sleep:
- Make sure that you push your tongue towards the tongue reservoir until the vacuum effect is felt. Dormio won't fall out of place as long as it is vacuumed with your tongue properly.
- Repeat the process if you feel that the vacuum effect is no longer available.
- Make sure that Dormio does not touch your pillow. In such a case, outside contact will cause the tongue vacuum to fail.
Dormio is only suitable to use by patients between ages of 18-70.
People with severe obstructive sleep apnea syndrome should not use Dormio without consulting their doctor. Dormio is not an equivalent of CPAP for severe apnea patients.
It is inconvenient for people who have the following diseases and conditions to use Dormio and they should never use Dormio.
- COPD
- Asthma
- Lung Cancer
- Heart Failure
- Cerebrovascular Disease
- Central Sleep Apnea Syndrome
- Temporomandibular joint dysfunction
- Excessive Gag Reflex
- Gum Disease
- Regular use of sedative medicine
No. Unlike some other products currently available in the market, Dormio is not disposible. Dormio is an intraoral appliance made of medical silicone. Since it has a constant contact with the mouth tissue during its use, we recommend 6-months usage period considering both the hygienic aspect and the rate of wear.
You can easily clean Dormio by soaking it in boiling water for 3-5 minutes. You can store Dormio in its protective case after cleaning.
Since we do not have any clinical data, we do not recommend to use Dormio for people who have other respiratory diseases such as asthma, COPD, etc.
Dormio falls in the category of products that are not suitable for return due to their contact with body fluid during use. Unpacked products will be considered as tried and returning will not be possible.
You may return unopened products for 14 days.
You can easily contact us through our Whatsapp support line: +90 555 010 55 65 or by sending an e-mail to info@respogadgets.com

 Live Sales Support !
Live Sales Support !